Introduction: Understanding the Crown Area in Hair Restoration
The crown, often referred to as the vertex, is one of the most complex and challenging areas in hair restoration surgery. Unlike the hairline, which focuses primarily on framing the face, the crown is a circular region where hair grows in a spiral or whorl pattern. This natural swirl makes surgical planning more intricate and technically demanding.
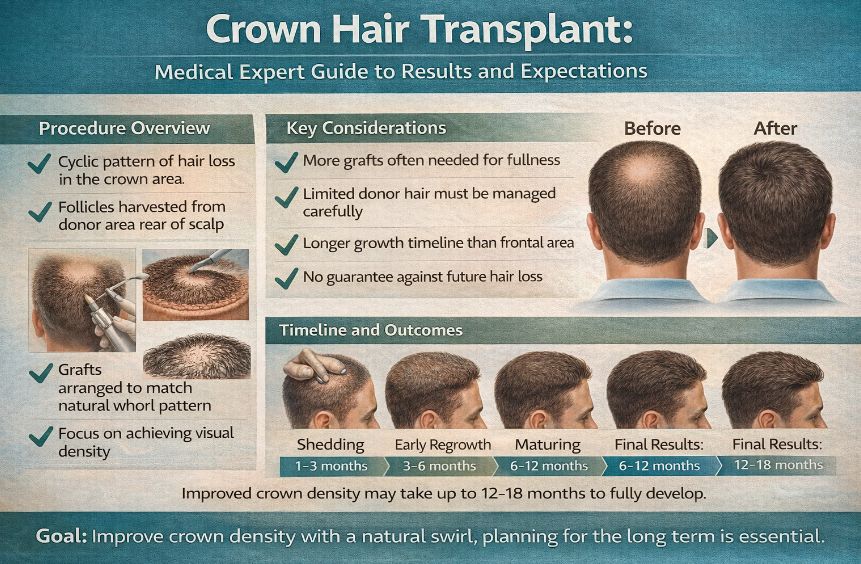
From a hair transplant specialist’s perspective, treating crown hair loss requires a different mindset than frontal or mid-scalp restoration. The direction of hair growth, the density requirements, and the long-term progression of hair loss all influence surgical decisions. Patients frequently underestimate how unique the crown is compared to other parts of the scalp, which can lead to unrealistic expectations if not properly educated beforehand.
A crown hair transplant is not simply about placing grafts; it is about recreating a natural flow, balancing density, and planning for the future.
Why the Crown Is Different from the Hairline
Hair loss in the crown typically follows a circular expansion pattern. As thinning progresses, the affected area widens outward rather than receding backward as seen in the hairline. This geometric difference has practical implications:
-
Surface Area: The crown can cover a larger area than it initially appears.
-
Density Requirements: Achieving visual coverage often requires more grafts.
-
Whorl Direction: Hair grows in a spiral, not straight lines.
-
Progression Uncertainty: Crown thinning may continue even after treatment.
Because of these factors, surgeons must balance artistry with long-term medical planning. Overly aggressive density early on can deplete donor reserves needed for future procedures.
Causes of Crown Hair Loss
The primary cause of crown thinning is androgenetic alopecia, also known as male or female pattern hair loss. This condition is driven by genetic sensitivity to dihydrotestosterone (DHT), which gradually miniaturises hair follicles. However, additional contributors may include:
-
Hormonal fluctuations
-
Chronic stress
-
Nutritional deficiencies
-
Inflammatory scalp conditions
-
Age-related follicle weakening
While a transplant addresses the visible thinning, understanding underlying causes helps maintain long-term results and manage expectations.
Who Is an Ideal Candidate for a Crown Hair Transplant?
Not every individual experiencing crown thinning is automatically a suitable candidate. Proper evaluation includes scalp examination, donor hair assessment, and long-term planning. Ideal candidates typically share several characteristics:
-
Stable or slowly progressing hair loss
-
Adequate donor density at the back and sides of the scalp
-
Realistic expectations regarding density
-
Good overall health
-
Willingness to consider medical maintenance therapies
Younger patients with rapidly progressing loss may be advised to wait or combine surgery with non-surgical treatments to stabilise the pattern before transplantation.
Donor Area Considerations
The donor region, usually located at the occipital scalp, contains hair follicles genetically resistant to DHT. These follicles are harvested and relocated to the crown. The quality of the donor area determines the success of the procedure.
Important donor characteristics include:
-
Hair thickness and calibre
-
Colour contrast between hair and scalp
-
Density per square centimetre
-
Curl or wave pattern
-
Elasticity of the scalp
A strong donor area allows for better coverage and flexibility in designing the crown swirl. Limited donor supply requires more conservative planning.
Techniques Used in Crown Hair Transplants
Two primary extraction techniques are commonly used:
Follicular Unit Extraction (FUE)
FUE involves removing individual follicular units using micro-punch tools. It leaves tiny, nearly invisible scars and allows for flexibility in harvesting patterns. This method is often preferred for crown work due to its precision and minimal downtime.
Follicular Unit Transplantation (FUT)
FUT involves removing a thin strip of scalp from the donor region, which is then dissected into grafts. It may yield a larger number of grafts in a single session but results in a linear scar. Some patients choose FUT when extensive coverage is required.
Both techniques can produce excellent crown results when executed by experienced surgeons. The choice depends on donor characteristics, graft requirements, and patient preference.
Designing the Crown Whorl
One of the most artistic elements of crown restoration is recreating the natural spiral. Each person’s crown swirl is unique, and improper angling can lead to unnatural appearance. Surgeons carefully analyse pre-loss photographs when available and study existing hair direction before placing grafts.
Key design principles include:
-
Maintaining natural hair angles
-
Gradual density transitions
-
Respecting the original swirl orientation
-
Avoiding abrupt directional changes
This meticulous approach ensures the transplanted hair blends seamlessly with surrounding native hair.
Graft Numbers and Density Expectations
Patients often expect the same density in the crown as in the frontal hairline. However, achieving full density in the crown requires significantly more grafts due to the circular pattern and visual exposure under overhead lighting.
Average graft requirements may range widely depending on the size of the thinning area. Visual density, rather than absolute density, is the primary goal. Strategic placement and angling often create the illusion of fullness without exhausting donor reserves.
The Healing and Growth Timeline
Hair growth after a crown transplant follows predictable biological phases:
-
Initial Healing (1–2 weeks): Redness and minor scabbing resolve.
-
Shedding Phase (1–3 months): Transplanted hairs fall out temporarily.
-
Early Regrowth (3–6 months): Fine new hairs begin to emerge.
-
Maturation (6–12 months): Hair thickens and blends naturally.
-
Final Results (12–18 months): Full texture and density become visible.
The crown often takes slightly longer to show final results compared to the hairline due to circulation patterns and growth direction.
Potential Risks and Considerations
Like any surgical procedure, crown hair transplantation carries potential risks, though they are generally minimal when performed by qualified professionals. These may include:
-
Temporary swelling or redness
-
Shock loss of surrounding hair
-
Uneven density during early growth stages
-
Minor scarring in donor areas
-
Prolonged shedding in rare cases
Careful pre-operative planning and adherence to post-operative instructions significantly reduce complications.
The Role of Medical Therapy
Non-surgical therapies can complement surgical results by stabilising ongoing hair loss. These may include topical or oral medications, low-level laser devices, or platelet-based regenerative treatments. Combining surgery with medical management often yields more sustainable outcomes.
Psychological Impact and Patient Satisfaction
The crown is less visible in daily interactions but becomes noticeable under bright lighting, photographs, or aerial views. Many patients seek treatment due to self-consciousness in professional or social settings. Restoring density in this region can significantly enhance confidence and self-perception.
However, satisfaction depends on realistic expectations. Understanding that crown density appears softer than frontal density is crucial to long-term happiness with the outcome.
Crown Transplant vs. Frontal Transplant Priorities
In many cases, surgeons prioritise the frontal hairline before addressing the crown. The hairline frames the face and has greater visual impact. Once the frontal area is stabilised and donor reserves are assessed, the crown may be treated in the same or a later session.
This staged approach ensures balanced allocation of grafts and preserves options for future needs.
Long-Term Planning and Future Hair Loss
Hair loss is progressive. A crown transplant does not halt future thinning of surrounding native hair. Therefore, long-term strategy is essential. Surgeons must anticipate potential expansion of thinning zones and preserve donor supply accordingly.
A well-planned procedure considers not just the current appearance but the patient’s likely hair pattern decades ahead.
Advances in Technology and Technique
Modern advancements such as high-magnification microscopes, robotic extraction tools, and refined graft handling techniques have improved survival rates and naturalness of results. Enhanced anaesthesia methods also contribute to patient comfort and quicker recovery times.
Final Assessment: Precision, Patience and Planning
A crown hair transplant is both a technical and artistic procedure requiring meticulous design, realistic expectations and long-term foresight. When performed by an experienced specialist, it can restore natural flow, improve visual density and significantly enhance confidence.
However, it is not an instant transformation. The crown demands patience, strategic graft allocation and sometimes combination with medical therapies for optimal outcomes. Patients who understand the biological timelines and density limitations are far more likely to appreciate the subtle yet meaningful improvements achieved through this specialised form of hair restoration.
